UB-founded company uses AI to assist surgeons treating brain

UB News Release, December 18, 2023, By Laurie Kaiser
(left: Vincent Tutino, CFO and UB biomedical engineering grad, Ciprian "Chip" Ionita, CEO & UB assistant professor of biomedical engineering, and Mohammad Mahdi Shiraz Bruwani, the grant's principal investigator and the company's chief technical officer. Photo: Douglas Levere )
BUFFALO, N.Y. — Brain, or intracranial aneurysms (IA), can lead to hemorrhagic strokes and are responsible for close to 500,000 deaths worldwide every year.
Despite advances in medical treatments, around 65% of patients with ruptured IAs die from the initial bleed or subsequent complications, noted Ciprian (Chip) Ionita, University at Buffalo assistant professor of biomedical engineering and neurosurgery. Among the survivors, about 50% become disabled with significant loss of independence.
Ionita, who also serves as director of the Endovascular Devices and Imaging Lab at Canon Stroke and Vascular Research Center (CSVRC), hopes to improve these odds through Quantitative Angiographic Systems. Artificial Intelligence (QAS.AI), a small biomedical engineering company he founded at the CSVRC in 2020.
Ionita and his research team are developing software intended to detect complications during surgery, such as inadequate blood flow in the brain, and forecast whether a selected treatment method will succeed — all in real time.
“The technology developed by QAS is fundamentally different than current FDA-approved AI solutions, which are used mostly for offline diagnosis or clinical workflow optimization,” Ionita said. “We are pushing the boundary of the AI applications, developing prognosis tools for the operating room, which could improve treatment outcomes and early detection of complications. This will cut health care costs and save lives.”
Now, Ionita and his team have the opportunity to apply their research to clinical evaluations in two sites in Buffalo and one in Florida, thanks to a $1 million, Phase II grant from the National Science Foundation’s (NSF) Small Business Technology Transfer (STTR) program.
Funding extends work to 2025
Located at UB’s New York State Center of Excellence in Bioinformatics and Life Sciences, QAS.IA integrates years of research by faculty and students in the Jacobs School of Medicine and Biomedical Sciences and the School of Engineering and Applied Sciences.
In 2021 QAS.AI received $256,000 in initial funding from the same NSF program to begin creating the AI-based software.
“The AI software we developed is integral during the intervention process, as it assesses the likelihood of aneurysm healing,” he said. “If it predicts a low probability of healing within a year, this information is immediately relayed to the neurosurgeons. This enables them to consider adjusting the treatment approach, potentially by incorporating an additional device. This feature is crucial for keeping a close watch on the patient’s condition, helping doctors respond effectively to changes in the aneurysm’s behavior.”
The new grant, which extends from fall 2023 to fall 2025, will fund the hiring of a company to develop clinical-grade software to translate the current software that QAS.AI is using to accomplish these goals.
“It will ensure that our software is HIPPA [Health Insurance Portability and Accountability Act] compliant, has patient protection and all the robustness required by clinical software,” Ionita said. “It has to be completely integrated with surgical equipment.”
Clinical evaluations in Buffalo, Florida
The grant is also funding clinical evaluations at the Gates Vascular Institute (GVI), Mercy Hospital of Buffalo and the University of South Florida’s Department of Neurosurgery and Brain Repair.
Ionita, who conceived the AI software, and is the QAS-AI chief executive officer, has engaged biomedical engineering students in a variety of projects to advance the technology. Mohammad Mahdi Shiraz Bhurwani, who served as the company’s lead AI scientist in summer 2021 while completing his doctoral research in the department, is now the grant’s principal investigator and the company’s chief technical officer.
Other team members include Jason Davies, assistant professor of neurosurgery and biomedical informatics, who serves as chief medical officer; Vincent Tutino, assistant professor of pathology and anatomical sciences, who serves as the chief financial officer; and two PhD candidates.
The platform for Phase II includes a fully automated method to identify the location and extent of the IA. It also allows for instantaneous extraction of the imaging biomarkers, prognosis of the surgical outcome at one-year post-procedure in a fraction of a second to allow neuro-interventionalist to readjust the endovascular therapy, and full integration with the angiographic systems regardless of the manufacturer, Ionita explained.
“When brain aneurysms become symptomatic and traditional treatments such as opening the skull prove ineffective, less invasive neuro-endovascular interventions can offer a solution,” Ionita said. “This can be accomplished by placing coils, stents or a combination of these devices in the region of an aneurysm.”
However, he said, they don’t always result in complete IA healing. In fact, between 70 to 80% of these AI cases are treated successfully while the other 20 to 30% require the patient to come back for additional procedures.
“We want to reduce this number of re-treatments to single digits, if possible,” Ionita said. “Our goal is to develop a technology that allows successful treatment in one stop.”
Potential commercial impact is ‘immense’
Ionita expects the first clinical evaluation at GVI to be operational by August 2024; evaluations at the other two spots will follow.
“Through the clinical evaluations, we will be preparing for clinical trials,” he said, adding that they will require future grants or private investments but should lead to FDA approval of the AI software.
The potential commercial impact of this technology is immense, Ionita said, especially at a time when medical imaging companies are seeking new innovations to maintain a competitive edge.
“By integrating an intraoperative software for informed decision-making, these companies could experience a 5% increase in scanner sales,” he said. “With over 6,000 hospitals in the U.S., each equipped with an average of six angiographic suites, this translates to projected revenue of $1.1 billion in U.S. markets.”
In addition, hospital and insurance company administrators will benefit from reduced re-treatment costs, which average $65,000 each and would amount to an annual savings of $1.95 billion in the United States alone, he said.
“This innovative AI platform promises to revolutionize the medical imaging and health care industries,” he said, “improving patient outcomes while boosting the bottom line.”
UB Neurosurgeons innovate new ways to attack blood clots
UB News Release, September 14, 2022, By Ellen Goldbaum
"UB neurosurgeons innovate powerful new ways to attack multiple blood clots deep in the veins of the brain"
BUFFALO, N.Y. – The University at Buffalo team that a decade ago helped usher in a new era in acute stroke treatment has turned its innovative approach to addressing the rare but potentially deadly phenomena when multiple blood clots strike deep in the veins of the brain.
“Typically, when we think of stroke, we think about blockages in the arteries to the brain,” said Elad Levy, MD, SUNY Distinguished Professor, L. Nelson Hopkins Chair of Neurological Surgery and chair of the Department of Neurosurgery in the Jacobs School of Medicine and Biomedical Sciences at UB. “But blockages can also happen in the deep veins of the brain.”
The condition is called cerebral venous sinus thrombosis (CVST), where a blood clot forms in the brain’s venous sinuses, preventing blood from draining out of the brain.
“In these very rare cases, when multiple veins are involved, the blood coming into the brain can’t drain out,” Levy said. “This causes the brain to swell in the skull, which can lead to hemorrhage.”
When a single clot in the brain is involved, the standard of care is to treat the patient with blood thinners. But, Levy said, cases of multiple clots in the veins of the brain require a more aggressive approach.
“If the patient falls into a coma, then you need to act fast and mechanically pull those clots out of the brain veins,” he said. “The faster you get in there to open up the vessels, the better the patient will do.”
When multiple major veins in the brain are obstructed, a phenomenon the UB team has seen more than a dozen times since 2009, including recently with COVID-19, the neurosurgeons have used mechanical thrombectomy to literally suck the clot out of the vein. The procedure is called venous thrombectomy.
“Venous thrombectomy is not truly standardized yet,” said Rosalind Lai, MD, who recently joined UB Neurosurgery as a fellow after completing her medical education at Harvard Medical School and residency at Brigham and Women’s Hospital. “There’s still active research into when and how it can be helpful for patients.”
And while Levy stressed that these phenomena are exceedingly rare, the UB team has treated two such cases in the past month in young, otherwise healthy individuals who had recently been infected with SARS-CoV2.
One of those patients continued to rapidly decline, even after several hours on a blood thinner.
“In that case, we really had no choice but to do the procedure,” said Lai, who assisted Levy in the operation. “The procedure went really smoothly. Dr. Levy is beyond words in terms of what he can do. He got in there very quickly and took the clot out.”
After the procedure, CT images showed that all the occluded veins had been opened up.
“And clinically, over the next few days, the patient continued to improve,” said Lai. “It was remarkable to see how this procedure made for such a life-changing event for this individual. Her case shows that there’s a definite need for more study on indications for venous thrombectomy. We need to be good at selecting the right patients for the procedure. She was certainly a great candidate for this.”
The next frontier
“This is the pivot point with stroke,” said Levy. “Learning how to treat vascular disease from the venous side versus the arterial side is the next frontier.”
It’s a frontier that the UB team is well-suited to explore.
“Whether it’s finding ways to expand the time window for treatment or adapting techniques from other disciplines, the mission of the UB Department of Neurosurgery has been to explore powerful innovations that will help more patients get back to normal life and function,” said Allison Brashear, MD, vice president for health sciences at UB and dean of the Jacobs School.
Led by L. Nelson “Nick” Hopkins, MD, SUNY Distinguished Professor and former chair of the UB Department of Neurosurgery, the team began pioneering new techniques back in the 1990s, using minimally invasive stroke treatments. These treatments take advantage of the body’s circulation system by threading micro-thin devices through an artery in the groin to reach blocked vessels in the brain, where they are then treated with stents.
Despite initial resistance to those innovations, the field has embraced them. Mechanical thrombectomy to remove arterial clots is now the established standard of care for certain types of acute stroke. The UB team is now using a similar minimally invasive approach to treat multiple blockages in the veins of the brain.
That mindset, focused on finding more ways to intervene even in the most severe situations, is again at work with the CVST cases, said Levy, who completed his fellowship under Hopkins in 2003, joined the UB faculty in 2004 and was named chair of neurosurgery in 2013.
“The ethos, the culture among UB neurosurgeons, is to push the envelope, to expand the landscape of stroke intervention, to develop and implement novel technologies to continue to provide cutting-edge care for increased patient populations,” said Levy, who is president of UBNS, the neurosurgery practice plan of UBMD Physicians’ Group.
Over the past dozen years or so, at Kaleida Health’s Gates Vascular Institute, where Levy is co-director of the Gates Stroke Center and Cerebrovascular Surgery as well as director of endovascular stroke treatment, he and his team have treated 20 cases where blockages occur in many or even all of the major veins of the brain. Some of these cases involved otherwise healthy young people, some of whom were recovering from COVID-19.
While the connection with COVID-19 is not yet clear, the UB researchers expect their ongoing studies of these clots and their access to those stored in UB’s Clinical and Translational Research Center biorepository will provide insights into how and why they occur.
Multidisciplinary endovascular expertise
Strong collaborations with the Endovascular Devices and Imaging Lab in the Canon Stroke & Vascular Research Center, located upstairs from the GVI, provide the neurosurgeons a critical tool in exploring how to treat endovascular disease including CVST.
Led by Ciprian N. “Chip” Ionita, PhD, assistant professor of biomedical engineering in the School of Engineering and Applied Sciences and the Jacobs School, the center focuses on creating 3D-printed phantoms of the body’s complex circulatory network so that surgeons can optimize their procedures before they head into the operating room.
“We subject all the devices to different patient anatomies in 3D-printed phantoms to see which one is better for a particular task,” he explained. “You can evaluate them in animal models but those don’t give you the ability to experience human anatomy, which can be very different in some people. There are these very tortuous pathways that have to be navigated all the way to where the clot is. You need to optimize the techniques in order to pull out those clots.”
Advances in the stents themselves are also playing a role, advances that in some cases are a direct result of the collaboration the UB team at the GVI has with the Jacobs Institute (JI), a nonprofit organization whose mission is to accelerate the development of next-generation technologies in vascular medicine.
The JI is located just upstairs from where the UB neurosurgeons perform the surgeries in the GVI/CTRC building that was specifically constructed to promote these kinds of collaborations between scientists, engineers and surgeons.
“We work very closely with the research engineers and scientists at the JI to provide feedback from these cases in real time,” said Levy, “so engineers can continue to work with the device companies to create second- and third-generation devices, making them bigger, longer and more supple.
“The technology is evolving, so now we can get bigger tubes farther and deeper into the brain,” Levy continued. “Stents are being made out of novel polymers, which allows them to be more flexible so they are better able to navigate and wind around the twists and turns of human vascular anatomy.”
Suction catheters are now as wide as the circumference of a pen or even a marker, Levy explained, which in some cases is double the diameter of earlier devices, making them much more powerful.
“The bigger the tube the greater is the suction power to get these massive clots out of there,” he said. “There is a lot of science and technology advancing these tools for stroke intervention. Now we are taking them to use them on the venous side, but they weren’t developed for this. We borrowed them from cardiology and other disciplines, and are adapting them.
“Our decades of experience in thrombectomy and in brain venous anatomy coupled with the sheer volume of neurointerventions that we do has resulted in UB Neurosurgery and the GVI becoming a center to which hospitals around the world refer their patients suffering from complex neurovascular disease,” said Levy.

These images show the arteries (red) and veins (green) in the brain of a recent patient with CVST.
Hopkins to receive Norton Medal, UB’s highest honor
UB News Release, April 26, 2019, By Sue Wuetcher
Hopkins to receive Norton Medal, UB’s highest honor, at commencement
L. Nelson Hopkins will receive the Norton Medal at the Jacobs School of Medicine and Biomedical Sciences’ commencement ceremony on May 3.
As one of the founding figures of endovascular treatment for neurovascular disorders, Hopkins has redefined the field of vascular neurosurgery in stroke management and lesion stenting. In the process, he has trained a new generation of neurosurgeons in catheter-based technology for minimally invasive neurosurgery. Hopkins’ innovations in endovascular surgery serve as the benchmark for therapeutic endovascular intervention.
An advocate of cross-specialty collaboration, Hopkins fostered the creation of UB’s Toshiba (now Canon) Stroke & Vascular Research Center. He also conceived a new way to organize the multidisciplinary treatment of vascular disease, working with experts from around the world to design the Gates Vascular Institute. Hopkins then recruited the necessary partners to bring it and the Jacobs Institute — a non-profit dedicated to accelerating the development of next-generation technologies in vascular medicine — to life.
He currently is chief scientific officer of the Jacobs Institute, after serving as chair of the Department of Neurosurgery from 1989-2013. He joined the UB faculty in 1975.
Hopkins has served on the board of directors of the American Association of Neurological Surgeons (AANS) and on the executive committee of the Stroke Council of the American Heart Association. A past president of the American Academy of Neurological Surgery, he is a former chairman of the scientific and annual meetings of AANS and the Congress of Neurological Surgeons, and of the Joint Section on Cerebrovascular Surgery.
The UB President’s Medal, first presented in 1990, recognizes “outstanding scholarly or artistic achievements, humanitarian acts, contributions of time or treasure, exemplary leadership or any other major contribution to the development of the University at Buffalo and the quality of life in the UB community.”


UB spinoff lands nearly $1 million in federal funding
UB News, Nov. 4, 2019, by Charlotte Hsu
Neurovascular Diagnostics was co-founded by a local entrepreneur who lost his wife to aneurysms
BUFFALO, N.Y. — In 2002, Western New York entrepreneur Jeff Harvey lost his wife and high school sweetheart, Carol Harvey, to two ruptured brain aneurysms.
Years later, he is honoring her memory by working with University at Buffalo engineering and medical researchers with the goal of preventing similar deaths.
Jeff Harvey is co-founder of Neurovascular Diagnostics, a UB spinoff company that is developing a low-cost blood test to screen high-risk patients for unruptured brain aneurysms — pathological bulging in blood vessels that can eventually burst.
In 2015, Meng and Tutino, then her PhD student, submitted a grant application to the Brain Aneurysm Foundation to conduct innovative research geared toward detection of unruptured aneurysms. The study was selected for funding, and by chance, through the fund honoring Carol Harvey.
After the announcement of the awards, Jeff Harvey and Meng sought each other out – not difficult, given that they were both in Buffalo.
Jeff Harvey found the funded research extremely interesting and convinced Meng, Tutino, and Snyder to start a company with the goal of translating their work into a technology that could be commercialized to help patients.
The team also includes Kerry Poppenberg, a UB PhD candidate in biomedical engineering who is not employed by Neurovascular Diagnostics but works on aneurysm research in Meng’s lab through a grant from the UB Center for Advanced Technology in Big Data and Health Sciences (UB CAT), with matching funds from the company.
Like Jeff Harvey, Poppenberg was inspired in part by a personal experience — the loss of her grandmother, an avid reader with many interests who volunteered for numerous organizations, ranging from a nursery school to a hospice program, after retiring from a job at an insurance company. She often cared for Poppenberg and Poppenberg’s siblings when they were kids.
“I took Dr. Meng’s class and I learned about the research she was doing,” Poppenberg says, regarding how she became involved in Meng’s lab. “My grandmother died of an aneurysm, so it appealed to me that this is a project that can help people.”
The screening that Neurovascular Diagnostics is developing with NSF support would look for signs of a brain aneurysm in patients’ blood cells. As Tutino explains, the thinking is that inflammation caused by a brain aneurysm may alter gene expression in cells, causing levels of some RNA molecules in the cells to rise, and others to fall. The company’s blood test — AneuScreenTM — would detect these differences. The NIH-funded research could further enhance the test by identifying biomarkers that could provide insight into how risky a patient’s aneurysm may be. (Read More)
Learn More
The screening that Neurovascular Diagnostics is developing with NSF support would look for signs of a brain aneurysm in patients’ blood cells.
Rudin is named SPIE Fellow for advancing medical physics
UB News Release, May 2, 2018, By Ellen Goldbaum
"Rudin is named SPIE Fellow for advancing medical physics to improve the diagnosis and treatment of stroke"
BUFFALO, N.Y. — Stephen Rudin, PhD, SUNY Distinguished Professor in the Department of Radiology in the Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo, has been named a Fellow of SPIE, the International Society for Optics and Photonics.
Rudin, who directs UB’s Division of Radiation Physics, is one of 73 major international figures in optics, photonics and imaging named SPIE Fellows this year. A faculty member since 1977, he is being recognized for his achievements in image-guided endovascular interventions and medical physics.
A pioneer in developing new technologies in medical diagnostics and interventional imaging, Rudin has been at the forefront of developing high-resolution X-ray imaging detectors, dose reduction methods, and endovascular devices such as asymmetric stents.
Rudin’s work has major theoretical and clinical implications for medical physics, biomedical engineering and diagnostic radiology, as well as an immediate impact upon patient diagnosis and care, particularly in cases of heart and brain treatment. A leader in advanced X-ray planar and tomography imaging in neuroimaging applications, he has been involved in further developing X-ray angiography and computed tomography (CT) for diagnosis and assessment of neurovascular diseases.
Working with colleagues in the Canon Stroke and Vascular Research Center (formerly the Toshiba Stroke Research Center), Rudin and his team have been developing imaging methods geared toward replacing invasive neurovascular surgical procedures for treating pathologies, such as aneurysms, with minimally invasive image-guided interventions.
With continuous funding from the National Institutes of Health and other sources since 1977, Rudin has led the development of prototype high-resolution, real-time imaging detectors for diagnosing neurovascular diseases. He also has spent much of his career developing techniques that will minimize radiation doses patients receive during procedures such as angiography and CT scans, while improving device guidance.
He has had consistent support from industry, including Toshiba and Canon, for developing new imaging techniques to improve diagnosis and treatment of stroke and related disorders, with some of the projects resulting in products distributed worldwide.
Rudin founded and directs UB’s Medical Physics Graduate program, one of only 41 such nationally accredited programs in the U.S., and he has advised more than 110 graduate students at UB and Roswell Park Comprehensive Cancer Center. His group has received numerous awards including first prizes for projects, such as the creation of patient-specific 3D phantoms for vascular procedure treatment planning and research, patient dose savings with region of interest fluoroscopy, automatic brightness control in digital fluoroscopy, evaluation of amorphous selenium for fluoroscopy, new approaches to quality assurance in digital radiography, and a variety of other projects.
Rudin also has held joint appointments in the UB departments of Neurosurgery, Physiology and Biophysics, Biomedical Engineering, Electrical and Computer Engineering, Mechanical and Aerospace Engineering; and Physics.
A consistent contributor to the SPIE Medical Imaging Symposium and the SPIE medical imaging community in general, Rudin's advocacy and commitment to the field have resulted in UB’s recognized prominence in medical imaging internationally.
The author of more than 500 publications including over 200 SPIE articles and presentations, he has been awarded four patents and has received numerous awards from other major scientific societies, such as the Radiological Society of North America and the American Association of Physicists in Medicine. At UB, he is the recipient of a Sustained Achievement Award, a Product Development Fund Award and the Stockton Kimball Award, the highest honor for a UB faculty member in the Jacobs School of Medicine and Biomedical Sciences.
Rudin and his family live in Williamsville, New York.


UB biomedical engineer uses 3D printing to enhance surgery
UBNow, Dec 14, 2018, by Gina Marie Ciappina
"UB biomedical engineer uses 3D printing to create brain and heart models to enhance surgery"
A UB team of biomedical engineers, neurosurgeons and cardiovascular interventionalists has developed a way to generate 3D prints of the human vascular system, giving surgeons pre-surgical, hands-on access to individual patients’ life-threatening vascular diseases in the heart and brain before any scalpels ever touch human skin.
Initiated by Ciprian “Chip” Ionita, assistant professor in the Department of Biomedical Engineering, and Adnan Siddiqui, professor of neurosurgery in the Jacobs School of Medicine and Biomedical Sciences, the method that creates 3D prints is already being used to better prepare doctors performing delicate surgeries to treat such conditions as stroke, aneurysms, cardiac arrest and congestive heart failure.
The 3D prints also are being used to train residents and medical students learning how to proceed with these delicate and often life-or-death procedures.
“The whole idea of these 3D-printed models is to not only mimic patient anatomy, but to also mimic some of their vascular mechanical properties,” says Ionita, whose Department of Biomedical Engineering is a joint department in the Jacobs School and the School of Engineering and Applied Sciences.
Before 3D printing, these lifelike models were costly, complicated to make and had to be shipped from Switzerland at a cost of more than $12,000 each. Now, each model costs about $100 and can be produced specifically for one patient. The number of models and their specifics suitable for 3D printing are endless — and can be custom-made to fit individual patients.
Ionita and Siddiqui began their 3D-printing research when the Clinical and Translational Research Center (CRTC), Gates Vascular Institute (GVI) and Jacobs Institute were created to place engineers, physicists and vascular surgeons all under one roof.
“We are now able to optimize our research by meeting every day and working together,” Ionita says.
Learn More
“Without human interrelation between the researchers and the surgeons, the meaningful medical work can’t be done. ” -Chip Ionita
New brain surgery innovation: Practice on a 3-D model
UB News, November 24, 2015
Adnan Siddiqui, vice chair of neurosurgery, was interviewed by CNBC about his success treating a brain aneurysm in a Western New York mother-of-three after using a 3-D printer to model the aneurysm. He said that about a year ago, the physicians and surgeons working at the Jacobs Institute thought about using the Stratasys printer, not just for general training, but for specific surgeries. "We said, 'Why can't we print out brain aneurysms on these models?' " Siddiqui said…."This is going to change the way we train physicians," Siddiqui said of 3-D replicas. "I think this is going to impact every aspect of medical care."

Radiology software developed at UB receives award
UB Now, Jan 8, 2015, by Sue Wuetcher
Software developed by UB researchers at the university’s Toshiba Stroke & Vascular Research Center has received a 2014 “Minnies” award from AuntMinnie.com, one of the top websites in the radiology community.
The Dose Tracking System (DTS) — marketed by Toshiba but developed by a research group led by Daniel Bednarek, professor of radiology — took first place as “Best New Radiology Software” for 2014. It debuted last March at the annual meeting of the American College of Cardiology.
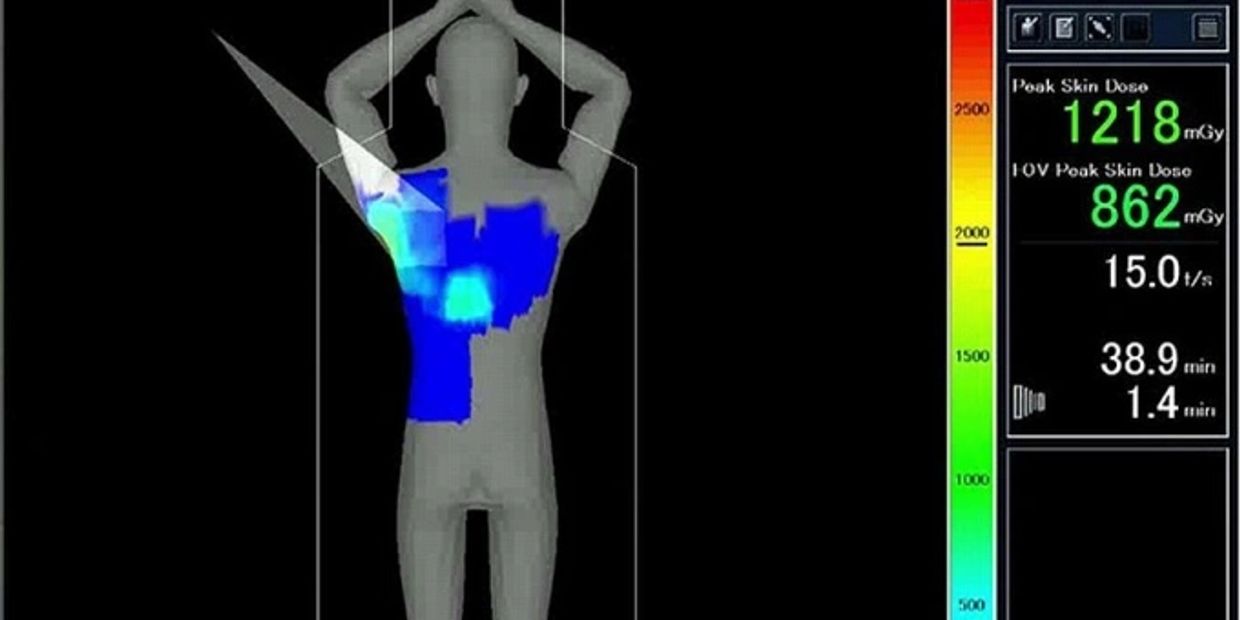
The DTS gives physicians a better idea of how much radiation patients are receiving during interventional fluoroscopic procedures, such as cardiac catheter ablation, vascular embolization and stent, filter or coil placement.
The DTS provides real-time data on the delivery of radiation during these interventional procedures via a detailed, intuitive, color-coded, 3-D map of the skin-dose distribution on a graphic of the patient. It highlights, with changing colors, if and when an area targeted to receive radiation should be changed to distribute the skin dose and minimize the chances of locally concentrated radiation exposure.
Learn More
The dose tracking system is the declared the
“Most Innovative Technology” at the 2012 meeting of the Radiological Society of North America.
UB granted $2.5M for image technology research
Buffalo Business First, Feb 20, 2013, by Dan Miner
A University at Buffalo researcher has received a four-year, $2.5 million federal grant to continue developing technology within a new class of image detectors.
The research of Stephen Rudin, director of UB’s Division of Radiation Physics, “has the potential to translate into manufactured medical systems providing new standards of care in neurovascular medicine,” according to a UB news release. The funding comes through the National Institutes of Health.
Rudin and other collaborators are furthering development of a high-resolution, region-of-interest X-ray imaging detector designed to provide better images while minimizing patients’ radiation doses.
The micro-angiographic fluoroscope (MAF) was designed by Rudin and his team during earlier phases of research. They recently achieved promising results after using the MAF to guide human interventions and will focus in the future on enhancing the detector system technology.
They plan to continue testing on patients as developments are implemented.
Rudin is joined by several UB collaborators, including Daniel Bednarek, professor of radiology, neurosurgery and physiology and biophysics; Dr. L. Nelson Hopkins, professor and chair of neurosurgery; Dr. Elad Levy, professor of neurosurgery and radiology; Dr. Adnan Siddiqui, associate professor of neurosurgery and radiology; Ciprian Ionita, researcher professor at the Toshiba Stroke and Vascular Research Center; Jihnhee Yu, associate professor of biostatistics in the School of Public Health and Health Professions.
Michael Silver, vice president for research at Toshiba Medical Research Institute USA, is also working on the project.
CTRC imaging center is devoted exclusively to research
UB News, July 1, 2013, by Ellen Goldbaum
"UB’s new CTRC imaging center is Western New York’s first devoted exclusively to research"
Imaging center provides researchers exclusive 24/7 access to some of the most powerful scanners available
BUFFALO, N.Y. – University at Buffalo biomedical researchers now have round-the-clock access to the most advanced imaging scanners available, as a result of four major acquisitions in the new imaging facility in UB’s Clinical and Translational Research Center (CTRC).
The new facility is Western New York’s first biomedical imaging facility dedicated exclusively to research.
“The new CTRC Imaging Center is a huge step forward for clinical research in Buffalo,” says Timothy F. Murphy, MD, CTRC director, senior associate dean for clinical and translational research at UB and SUNY Distinguished Professor in the UB School of Medicine and Biomedical Sciences. “It is an excellent resource for investigators at UB and Roswell Park and a powerful tool allowing researchers in the Buffalo Translational Consortium to perform state-of-the-art imaging studies.
“It’s also a huge recruiting tool,” he says. “State-of-the-art imaging has become an increasingly important element of translational research. Modern imaging techniques now provide information that previously could only be obtained from biopsies or autopsies. Many leading translational researchers have made imaging a critical aspect of their research.”
John M. Canty, Jr., MD, the Albert and Elizabeth Rekate Professor of Medicine has been appointed director of the CTRC Imaging Center, located in the CTRC on the Buffalo Niagara Medical Campus (BNMC). Robert Zivadinov, MD, PhD, UB professor of neurology and director of the Buffalo Neuroimaging Analysis Center, has been appointed the center’s director of magnetic resonance imaging (MRI).
Among the new center’s capabilities are:
- 9.4 Tesla Bruker MRI (Tesla indicates the strength of the magnetic field it generates)
- 3 Tesla Toshiba MRI
- Positron emission tomography/computing tomography (PET/CT)
- CT
Now, researchers at UB and partner institutions on the BNMC will have a total of four new state-of-the-art scanners at their disposal that are devoted exclusively to clinical and preclinical research. (Full Article)
Stroke center lands $15.8M deal with Toshiba
Buffalo Business First, March 9, 2012
An “unbelievable” $15.8 million commitment for new equipment and support from Toshiba Corp. will allow the University at Buffalo to expand its Toshiba Stroke Research Center this spring.
The commitment from Toshiba. includes $7 million in new imaging equipment, plus service and research support for 10 years valued at $8.8 million.
“This package is almost unbelievable, in terms of all the cool stuff that’s happening here,” says Dr. L. Nelson Hopkins, co-director of the center and chairman of the neurosurgery department in UB’s School of Medicine and Biomedical Sciences. “When people come from other places to see it, it knocks them off their feet.”
Doug Ryan, vice president of marketing and strategic development at Toshiba America Medical Systems in California, says Hopkins and his team at the Toshiba Stroke Research Center have made tremendous strides, and the company is eager to continue supporting those efforts. “I think we’ve changed the paradigm of stroke treatment here in the United States, at least,” he says. “It really is a tremendously exciting opportunity the team has created there,” he says. “I really think it’s going to be a world-class center in the United States.”
The Toshiba Stroke Research Center will move from its current home at Millard Fillmore Suburban Hospital to the top floor of the new Clinical and Translational Research Center, which is set to open in May on the Buffalo Niagara Medical Campus in a shared building with Kaleida Health’s Gates Vascular Institute. Much of the imaging equipment installed in recent weeks on the lower floors of the building in Kaleida’s GVI are also Toshiba machines. Ryan says the concept of the building is recognized as revolution-ary and is probably a model of how health care will be delivered in the future.
“It’s something that we believe is really the model of the future and that’s the main reason we’re so interested in supporting it,” he says.
Hopkins says having the Toshiba center in the same building as the GVI and the CTRC is key, as researchers can advance their work and test it without ever having to leave the building. “We’re developing new ideas and innovations and learning how to use them on patients, and training physicians and scientists on how it gets used,” he says. “Then if we need to test it further, we can take it right upstairs to the Toshiba Stroke Research Center.”
The new equipment from Toshiba will be installed this summer, including two biplane angiography machines; a 3T MRI (3 Tesla magnetic resonance imaging) unit; a 320-slice computed tomography (CT) scanner; and advanced ultrasound equipment.
Co-founded by Hopkins in 1997 with a $3.6 million gift from Toshiba, the research center was designed as a place where researchers from different disciplines could collaborate on stroke research. Toshiba has contributed a total of $25.8 million over the past 13 years. Hopkins is considered a superstar in the neurosurgery world and has developed a reputation based on his innovations in minimally invasive surgical techniques to treat aneurysms and stroke.
The Toshiba Stroke Research Center focuses on research related to the prevention and treatment of vascular disease through minimally invasive techniques.
Hopkins and his team have formed a series of strategic alliances with local, national and international partners to advance their research. Advances to date in imaging optimization have also led to potential new advances in device design, which in turn have presented new opportunities for hemodynamic investigation.
Recent successes touted on the center’s website include the development of a micro-angiographic fluoroscopy system that shows detail at the site of neurological intervention two to three times more clearly than imaging equipment now in use. The team is now working to make the system operator-friendly.
In addition to Toshiba, research at the center has been supported by federal grants from the National Institutes of Health. That includes the National Institute of Neurological Disorders and Stroke; the National Heart, Lung, and Blood Institute; the National Institute of Biomedical Imaging and Bioengineering; and the National Science Foundation.
